Lumbosacral Stenosis (LSS)
Lumbosacral stenosis (LSS) is a spinal disease characterized by the narrowing of the vertebral foramen and/or vertebral canal that can be aggravated by prolonged physical stress and activity in dogs. Multiple studies have reported the German Shepherd to be one of the most common breeds to be affected by LSS, in part because this breed has an increased prevalence of congenital anomalies affecting this region of the vertebral column.
The Patient
A 19-month-old female working German Shepherd dog (GSD) was presented with intermittent and shifting pelvic limb lameness. This had been noted by the owner since she was a puppy and was starting to be more frequent and severe. She was evaluated by her primary veterinarian and had sedated pelvic limb radiographs taken which revealed mild muscle atrophy but normal osseous structures. Otherwise considered healthy. The neurologic examination was considered normal. However, there was consistent discomfort noted on dorsiflexion of the tail.
The dog underwent a caudal lumbar vertebral column MRI using the Hallmarq small animal 1.5T machine (see Fig 1 and 2).
The Imaging Results
- Fig 1 A sagittal STIR view of the lumbar and lumbosacral vertebral column. The intervertebral discs are hydrated being T2 weighted hyperintense and showing normal shape and position within their respective disc spaces. There is no evidence of extradural, intradural, or intramedullary lesions affecting the spinal cord.
- Fig 2 (A) A transverse T1W view at the level of the L7-S1 disc space. There is no protrusion of the dorsal annulus of the disc (blue arrow) and the vertebral canal demonstrates normal epidural fat signal without displacement of the dural sac or nerve roots of the cauda equina (green arrow). There is mild to moderate bilateral foraminal stenosis (red arrows) noted with some loss of the perineural fat signal in association with subjectively enlarged articular processes (red stars) at this level. No contrast enhancement was noted on further imaging sequences.
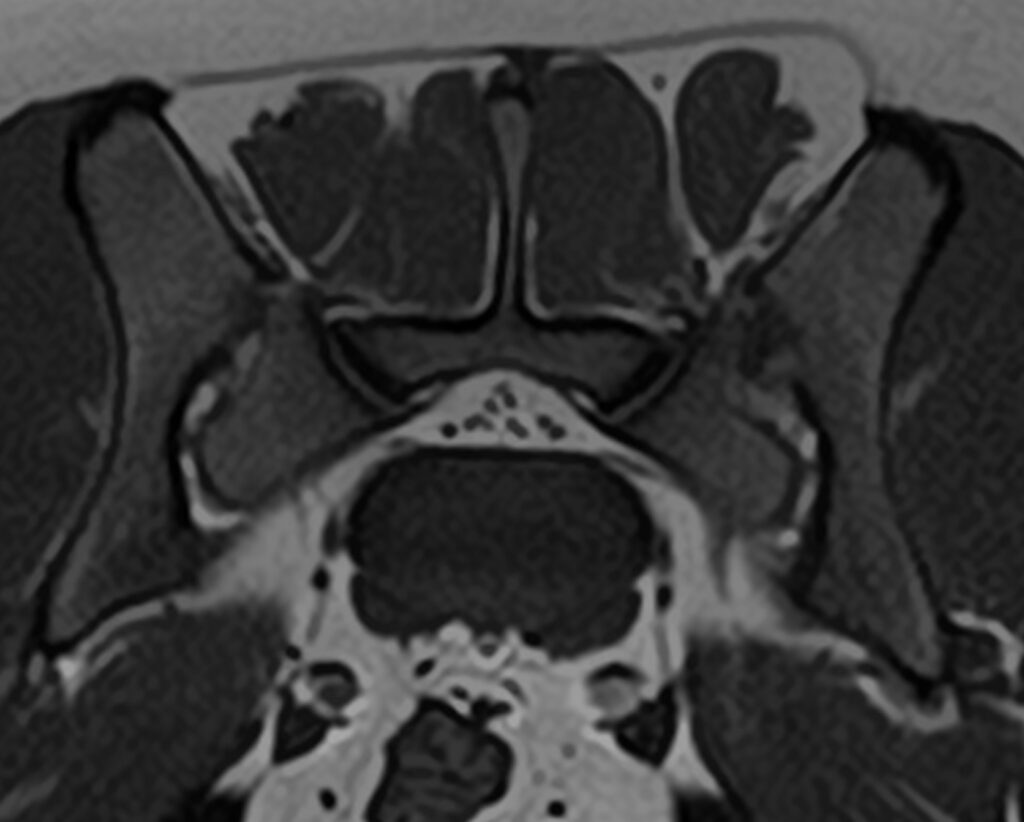
- Fig 2 (B) A transverse T1W view of a similarly aged GSD at the L7-S1 disc space. This image is shown as a comparison and is considered normal. The width of the bilateral foramen is notably larger with perineural fat signal throughout.
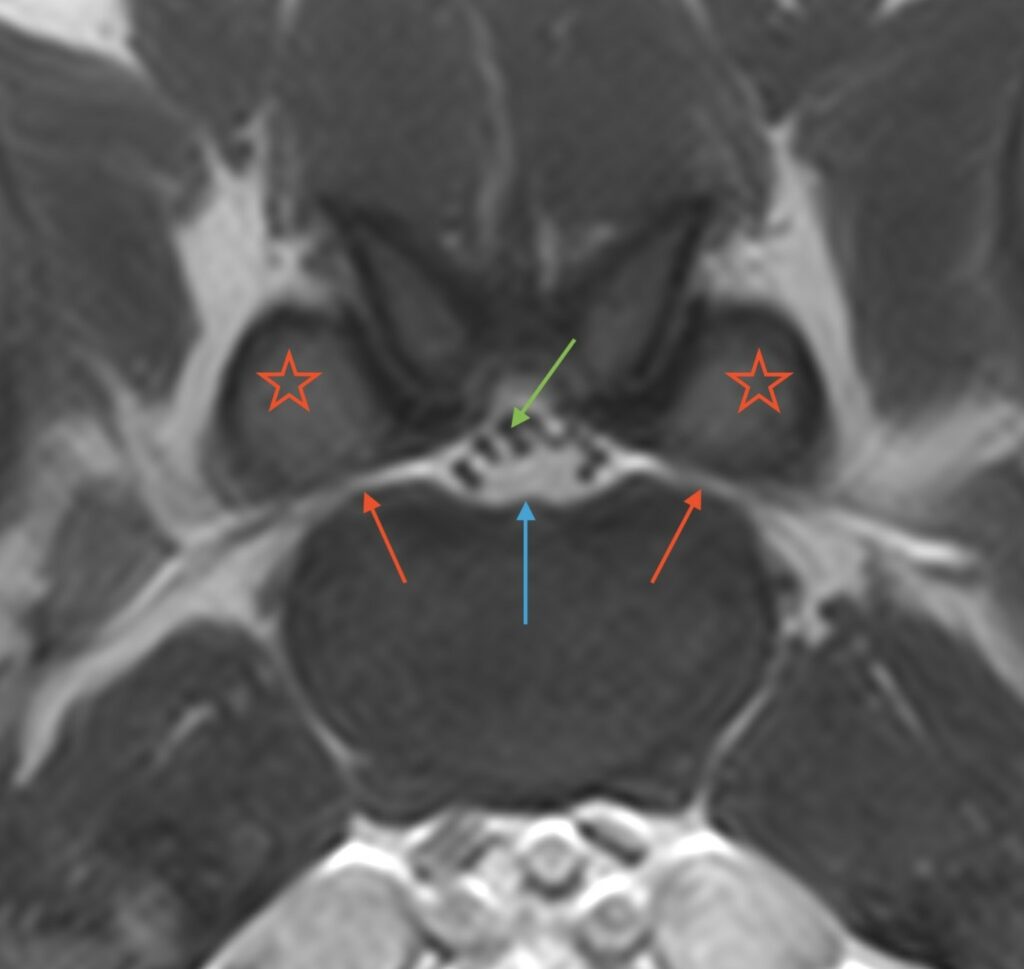
Based on these images, the dog was diagnosed with bilateral lumbosacral foraminal stenosis associated with subjectively enlarged articular processes. A dynamic CT study of this region could be valuable in such a dog to assess the osseous boundaries of the foramen in neutral and flexed views, which may be helpful to determine appropriate surgical therapy and enable measurement of structures for implant placement if this is necessary.
Disease Overview
Multiple studies have reported the German Shepherd to be one of the most common breeds to be affected by Lumbosacral stenosis (LSS), in part because this breed has an increased prevalence of congenital anomalies affecting this region of the vertebral column.
MRI Where Radiographs Fail
Radiographs do not allow accurate evaluation of intervertebral foraminal dimensions due to the superimposition of the articular processes of L7 and S1, particularly in patients with degenerative changes. With the widespread availability of magnetic resonance imaging (MRI), recognition of L7–S1 foraminal stenosis, and compressive radiculopathy of the L7 nerve root has increased dramatically.
MRI is the most sensitive imaging modality for the detection of soft tissue and nerve root lesions associated with LSS. Meticulous positioning of the animal and a 1–2 mm slice protocol are important to avoid partial-volume artifacts and false-positive findings when imaging the foramina with MRI as side-to-side comparison is a critical step in evaluation. The dog should be positioned in dorsal recumbency with the lumbosacral junction in extension to maximize diagnostic sensitivity.
Surgical Procedures for Lumbosacral Stenosis (LSS)
Several surgical procedures specifically addressing foraminal stenosis have been described. Surgical decompression of the L7 nerve root can be achieved by dorsal and medial approaches, mostly as an extension of the standard L7-S1 dorsal laminectomy with or without facetectomy. However, problems and complications of these procedures include limited access to lateralized intraforaminal compressions, postoperative hypermobility, and occasionally fractures of the contralateral articular process. As a result, alternative strategies for L7 nerve root decompression have been developed. One procedure involves a lateral foraminotomy, specifically targeting compressive lesions within the middle and exit zones of the NF.
Alternatively, several surgical distraction-fusion techniques aimed at distracting the L7-S1 intervertebral junction and thereby the L7-S1 NF have been described, potentially providing more long-term success.
With thanks to Dr. Baye Williamson DVM, DACVIM (Neurology) at Veterinary Emergency + Referral Center (VERC), Hawaii, for providing this case study.
References
- Seiler GS, Häni H, Busato AR, Lang J. Facet joint geometry and intervertebral disk degeneration in the L5-S1 region of the vertebral column in German Shepherd dogs. Am J Vet Res. 2002 Jan;63(1):86-90
- Smolders LA, Knell SC, Park B, Pozzi A, Meij BP, Steffen F. The effects of foraminotomy and intervertebral distraction on the volume of the lumbosacral intervertebral neurovascular foramen: An ex vivo study. Vet J. 2020 Feb;256:105435.
- Worth A, Meij B, Jeffery N. Canine Degenerative Lumbosacral Stenosis: Prevalence, Impact And Management Strategies. Vet Med (Auckl). 2019 Nov 19;10:169-183.


