Severe Osteoarthritis of the Distal Interphalangeal Joint
We look at the use of multi-modal imaging in helping diagnose severe osteoarthritis of the distal interphalangeal joint in an 8-year-old Belgian warmblood. Presenting with left forelimb lameness, the lameness improved following both an abaxial sesamoid nerve block and intra-articular anesthesia of the distal interphalangeal joint.
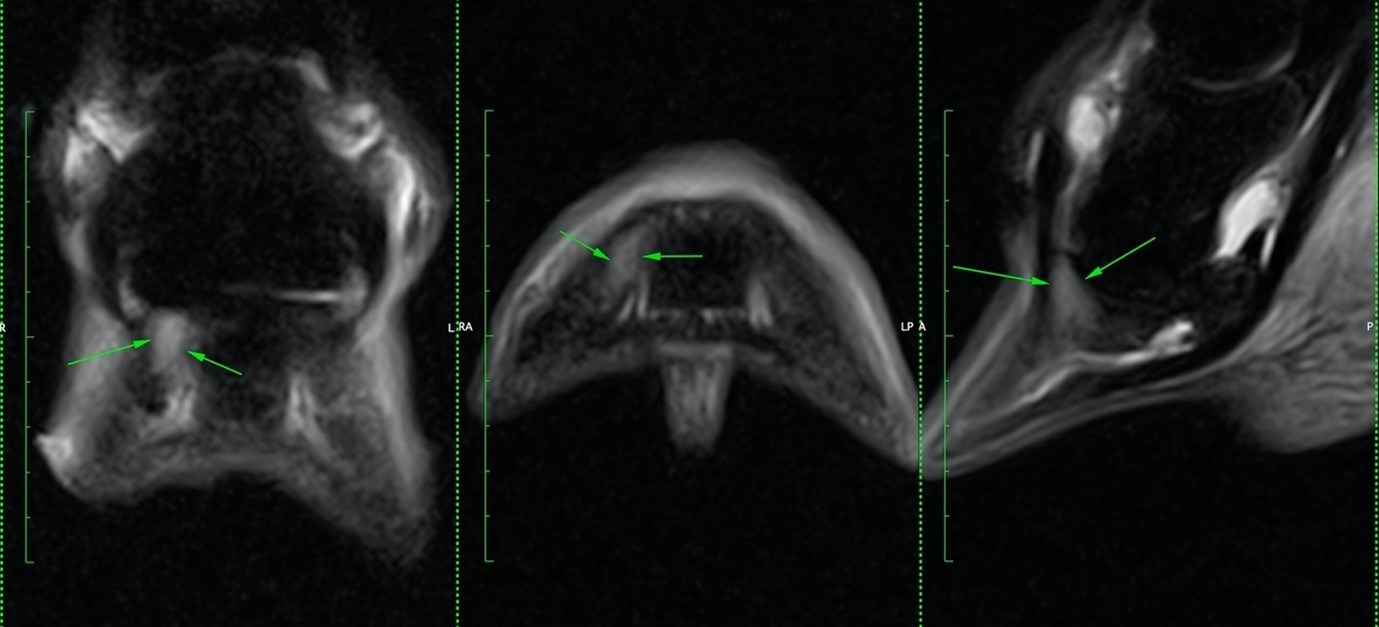
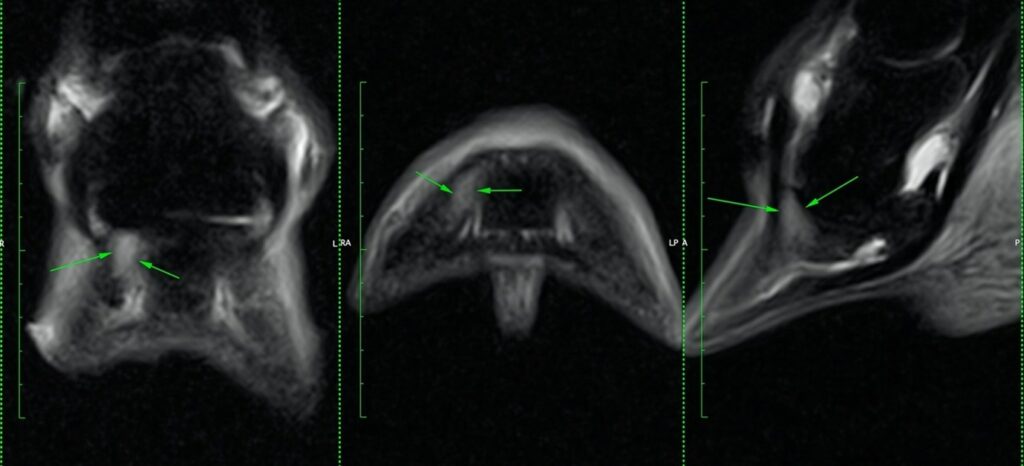
MRI Findings
A Standing Equine MRI of the foot revealed large sclerotic osteophytes on the medial and lateral aspects of the joint. At the extensor process of the distal phalanx, there was significant bone edema, sclerosis, and fragmentation of a large osteophyte at its tip (Figure 1). There was focal loss of the bright cartilage signal over the lateral condyle of the middle phalanx and a more extensive disruption of the normal signal on the medial weight-bearing surface of the distal phalanx (Figure 1), indicating cartilage injury.
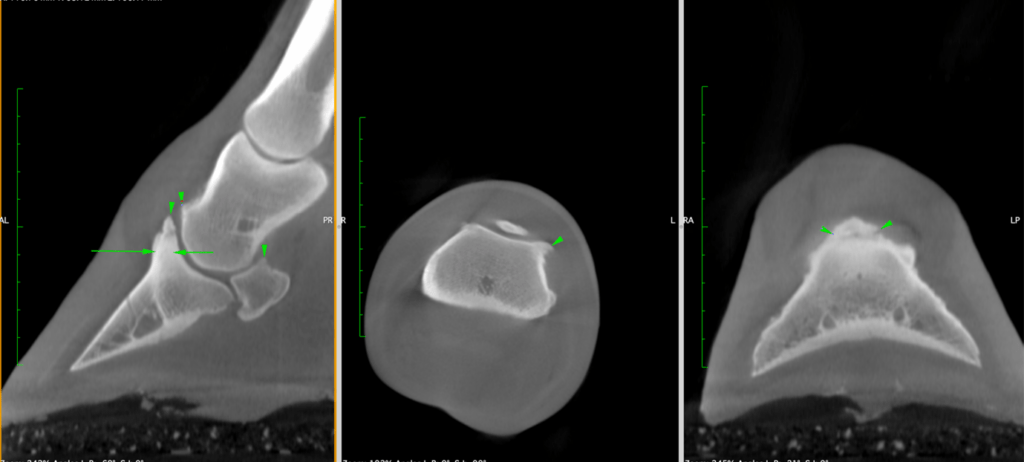
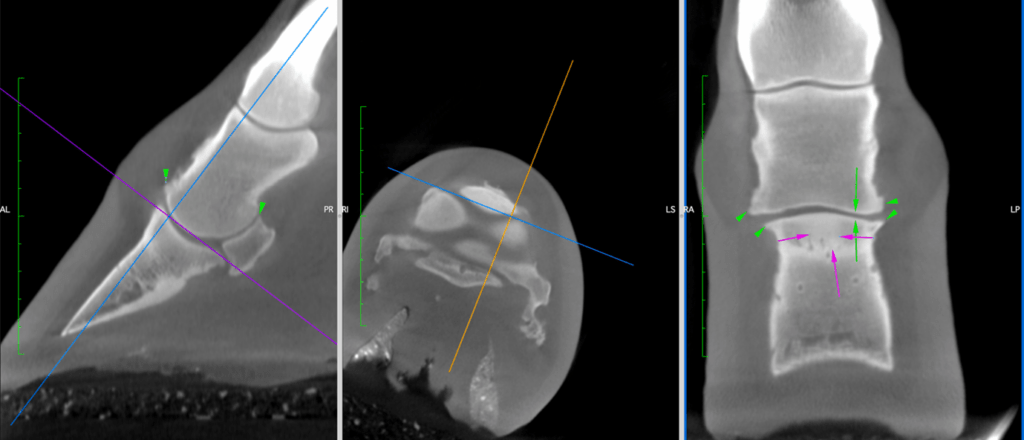
CT Findings
Additionally, a CT scan showed joint space narrowing in the lateral part of the distal interphalangeal joint (Figure 3) and provided a clear view of the extensor process fracture and new bone formation (Figure 2).
Conclusion
The combination of Standing Equine MRI and Vision CT provided a thorough assessment of the pathology. MRI revealed significant bone edema and cartilage injury. In addition, CT clearly demonstrated osseous abnormalities such as joint space narrowing, the extensor process fracture, and new bone formation. Importantly, this case highlights how, when used together, standing CT and MRI provide complementary information for the most accurate diagnosis and treatment planning.
With thanks to
Dr Sarah Taylor (BVM&S MSc PhD Cert ES(Orth) DipECVS DipECVSMR MRCVS)
Senior Lecturer in Equine Orthopaedics and team at The Royal (Dick) School of Veterinary Studies, for providing this case.