Cross-sectional imaging is becoming increasingly accessible and is very useful for the diagnosis of canine intervertebral disc extrusion (IVDE). However, when compared to computed tomography (CT), the use of magnetic resonance imaging (MRI) provides valuable information to support perioperative decision making.
In this post, guest author Daniel Low BVetMed CertAVP(GSAS) PGCertVPS MRCVS, RCVS Advanced Practitioner in Small Animal Surgery and ECVS Resident in Small Animal Surgery, reviews the current evidence and presents two case studies where MRI proved invaluable for perioperative decision-making in dogs suffering with thoracolumbar intervertebral disc extrusion (IVDE).
Diagnosing thoracolumbar intervertebral disc extrusion
Thoracolumbar IVDE may be diagnosed with myelography, noncontrast CT, CT-myelography, or MRI. The use of myelography is becoming less widespread with the increasing availability of cross-sectional imaging. Diagnostic sensitivity of noncontrast CT is at least 81%, and up to 100% in chondrodystrophic dogs with mineralised nuclei. If non-mineralised, the extradural compressive material can be visualised with CT-myelography with a sensitivity of up to 97%. Accordingly, superior anatomical definition is offered by MRI, with a sensitivity of 98.5%, and with avoiding subarachnoid contrast injection as another benefit.
Surgical planning for IVDE
The use of MRI affords better visualisation of extradural compressive material compared to CT-based techniques, where non-mineralised nuclear material and haemorrhage are not easily identifiable. Interestingly, while a larger hemilaminectomy window is not necessarily better, MRI provides more detailed information with which to plan the laterality, location, and extent of decompressive surgery.
Spinal cord contusion and swelling are also readily identifiable on MRI, and adjunctive procedures such as durotomy or extensive hemilaminectomy and durotomy may be considered. Nonetheless, it remains uncertain whether these adjunctive procedures improve the rate of recovery of ambulation and reduce the rate of progressive myelomalacia (a rare but fatal consequence of severe spinal cord injury).
The degree of intervertebral disc degeneration can be precisely assessed on MRI, whereas this is not possible on CT. In situ intervertebral discs with more advanced chondroid degeneration are at higher risk of subsequent extrusion, and targeted prophylactic fenestration of higher risk discs may be considered.
Prognosticating severe spinal cord injury
Decompressive surgery is generally associated with a good prognosis in dogs with thoracolumbar IVDE as long as deep pain perception is retained, whereas only 50-60% of dogs with loss of deep pain perception go on to recover independent ambulation after decompressive surgery. Certain MRI findings such as T2-weighted intramedullary hyperintensities may suggest an increased risk of a poor outcome, namely failing to recover ambulation or development of progressive myelomalacia.
Non-routine MRI sequences such as T2*-weighted or Half-Fourier-Acquired Single-shot Turbo Spin Echo sequences may also provide useful information for surgical decision-making. Respectively, gradient-echo signal voids and a greater craniocaudal extent of cerebrospinal fluid attenuation each may suggest that the dog is at an increased risk of progressive myelomalacia despite decompressive surgery.
Decompressive surgery is neither benign nor inexpensive. In dogs with high grade spinal cord injury, many owners are unwilling or unable to consent to decompressive surgery because of the associated aftercare commitments and the uncertain postoperative outcome. Many owners appreciate the additional prognostic information offered by MRI before making these major decisions.
Post-operative management of IVDE
Postoperative neurological deterioration unfortunately occurs in a minority of dogs after decompressive surgery. This may be due to progressive spinal cord contusion, residual extradural compression, de nouveau extrusion or haemorrhage, or iatrogenic spinal cord manipulation. The cause of postoperative neurological deterioration cannot be determined from the neurological examination and postoperative MRI is invaluable in the management of these cases.
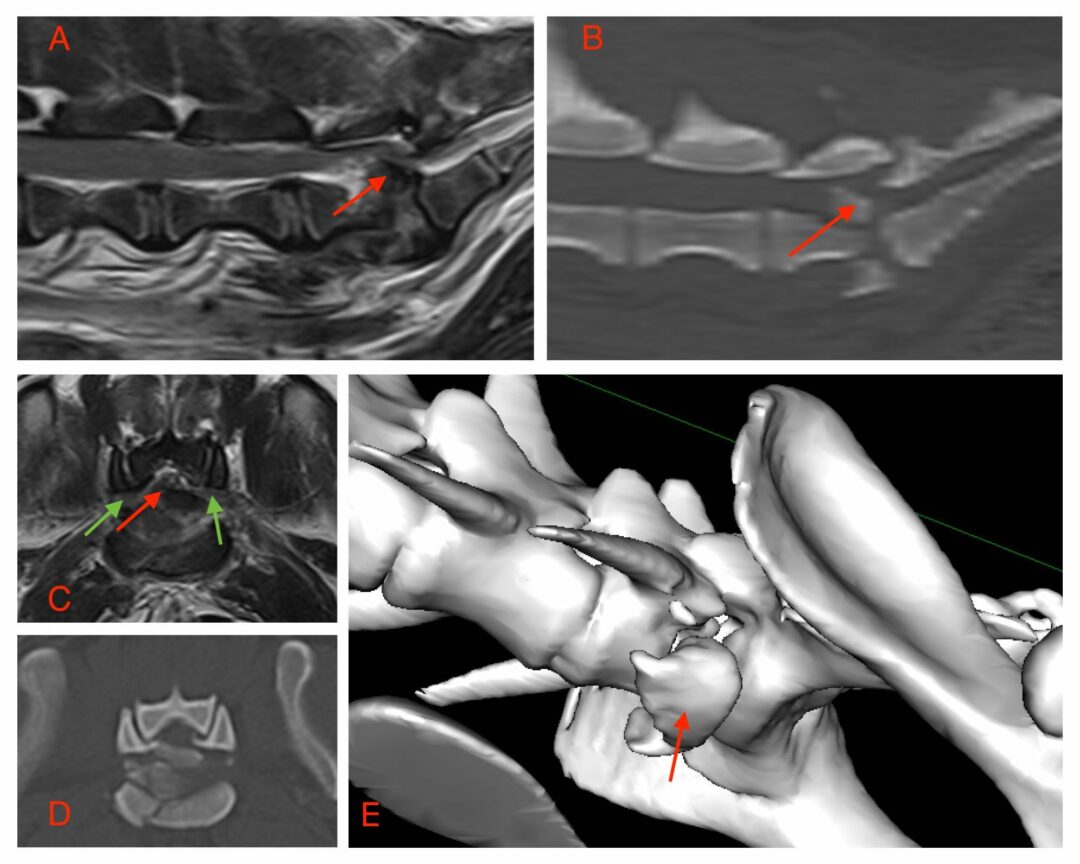
Case Study 1 – Dora
A five-year-old female neutered Miniature Dachshund (“Dora”) was presented with a seven-day history of lethargy progressing to paraplegia in the 24 hours prior. The neurological examination localised to the T3-L3 spinal cord segment. Deep pain perception was absent. A T11-T12 intervertebral disc extrusion was diagnosed on MRI of the thoracolumbar spine (Figure 1). T2-weighted intramedullary hyperintensity was noted cranial and caudal to the compressive lesion, which most likely represented spinal cord oedema. Dora’s owners consented to decompressive surgery after a discussion of prognostic outcomes and the risk of progressive myelomalacia. A right-sided T11-T12 hemilaminectomy was completed without complication to decompress the spinal cord. Recovery from anaesthesia was uncomplicated and Dora was discharged routinely after approximately four days in hospital.
Unfortunately, Dora failed to recover ambulation or deep pain sensation at the 12-week postoperative follow-up examination. Despite the disappointing outcome, Dora’s owners had been appropriately counselled and were prepared for this eventuality.
Case Study 2 – Luna
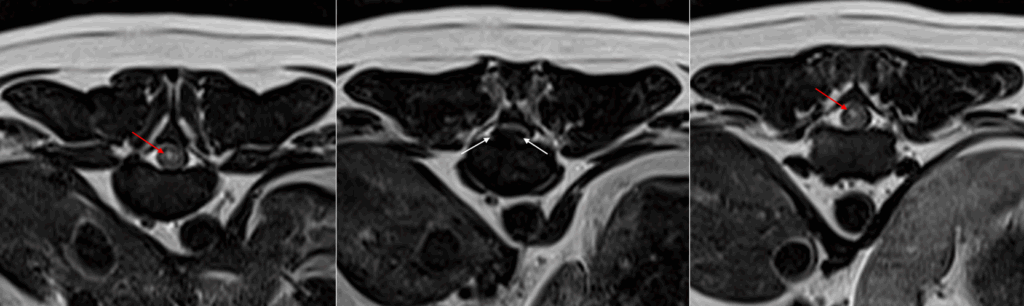
A six-year-old female neutered Miniature Dachshund (“Luna”) was presented with two days of lethargy progressing to ambulatory paraparesis in the 24 hours prior. The neurological examination localised to the T3-L3 spinal cord segment. A T13-L1 intervertebral disc extrusion was diagnosed on MRI of the thoracolumbar spine. A right-sided T13-L1 hemilaminectomy was completed without complication to decompress the spinal cord. Recovery from anaesthesia was uncomplicated.
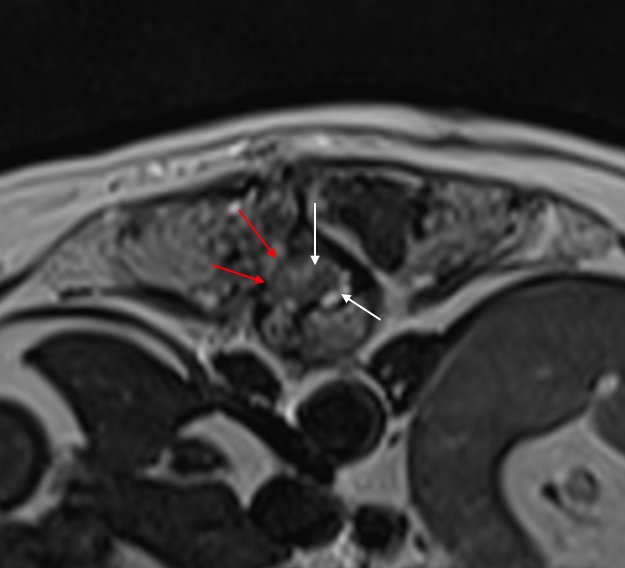
Unfortunately, Luna experienced postoperative neurological deterioration and became paraplegic with absent deep pain sensation 24 hours postoperatively. Repeat MRI was performed, which showed de nouveau extradural compressive material at the same level but on the contralateral side (Figure 2). A left-sided T13-L1 pediculectomy was performed to relieve the extradural compression and preserve vertebral column stability. Repeat MRI provided valuable information as to the cause of the postoperative neurological deterioration and allowed precise planning of revision surgery.
References
Olby NJ, Moore SA, Brisson B, et al. ACVIM consensus statement on diagnosis and management of acute canine thoracolumbar intervertebral disc extrusion. J Vet Intern Med. 2022;36(5):1570-1596. doi:10.1111/jvim.16480
Noyes JA, Thomovsky SA, Chen AV, et al. Magnetic resonance imaging versus computed tomography to plan hemilaminectomies in chondrodystrophic dogs with intervertebral disc extrusion. Vet Surg. 2017;46(7):1025-1031. doi:10.1111/vsu.12700
Jeffery ND, Mankin JM, Ito D, et al. Extended durotomy to treat severe spinal cord injury after acute thoracolumbar disc herniation in dogs. Vet Surg. 2020;49(5):884-893. doi:10.1111/vsu.13423
Low D, Vallios V, Basto T, Charalambous M. Longitudinal Assessment and Cost-Benefit Analysis of Prophylactic Fenestration in Chondrodystrophic Dogs With Follow-Up Magnetic Resonance Imaging. J Vet Intern Med. 2025;39(4):e70191. doi:10.1111/jvim.70191
Clark R, Ferreira A, Behr S. Significance of intramedullary T2* signal voids in the magnetic resonance imaging of paraplegic deep pain-negative dogs following intervertebral disc extrusion at short-term follow-up. Front Vet Sci. 2023;10:1248024. Published 2023 Sep 13. doi:10.3389/fvets.2023.1248024
Gilmour LJ, Jeffery ND, Miles K, Riedesel E. SINGLE-SHOT TURBO SPIN ECHO PULSE SEQUENCE FINDINGS IN DOGS WITH AND WITHOUT PROGRESSIVE MYELOMALACIA. Vet Radiol Ultrasound. 2017;58(2):197-205. doi:10.1111/vru.12463