When every second counts, accurate diagnostic information from shortened MRI protocols obtained early in the presentation of an emergency can drastically impact clinical outcomes and costs, for both the veterinary facility and the pet owner. Hallmarq Small Animal Advisory Board Member, Dr Catherine Love DVM, weighs up the cost to both clinic and client when choosing to use MRI short protocol over more traditional imaging methods.
MRI: the optimal imaging option
MRI is very effective at detecting soft tissue pathology whether the disease is in the brain, spinal cord, thorax, or abdomen. Historically, its high costs, lack of availability, and longer imaging times have limited its usefulness even when it is the optimal imaging option. In comparison, Computer Tomography (CT) is often the first choice in human emergency medicine due to its availability and short turnaround, even when it is not the optimal imaging choice. Similarly, in veterinary medicine, radiographs are often the diagnostic tool of choice because of availability, turnaround time, costs, and ease of training staff to perform.
If an MRI could be as efficient and cost-effective as radiographs, clinicians would likely prefer it based on its improved prognostic value alone, especially for cases where radiographs are not the optimal test.
MRI: cost savings for clinic and client
Shorter (10-15 minute) MRI protocols could be incorporated into emergency medicine to enable scanning of virtually all patients as conveniently and easily as performing radiography. Such abbreviated scanning protocols would only require simple injectable propofol-type anesthesia compared to general anesthesia. This not only removes the logistical barriers but also some financial barriers. Increasing the frequency of use and the volume of scans per week expedites the time to recover the cost of investment (purchase of MRI).
MRI: for managing clinical conditions
The indications for emergency MRI include clinical conditions in which the management options may differ between a surgical intervention versus less aggressive treatment plans. Typically, emergency clinical conditions that would benefit from MRI include:
- Pulmonary thromboembolism
- Feline Aortic Thromboembolism
- Multi-trauma particularly with head trauma, concern for internal bleeding
- Hemoabdomen/Hemothorax
- GI foreign body particularly involving radiolucent material. MRI can view organs that may be obscured by bone or foreign bodies on conventional X-rays or CT scans. It is capable of showing tissues from multiple viewpoints and is a noninvasive way to evaluate blood flow although the function of small and large bowel should be evaluated with a concurrent abdominal ultrasound
- Stroke or cardiovascular events
- Abnormal mentation with no history of trauma or toxin ingestion
- Neoplasia particularly for bleeding tumors or end-of-life decisions
- Seizures
- Urethral and ureteral blockages
- Spinal cord injuries
- Acute and Chronic pancreatitis: MRI is more sensitive than CT or ultrasonography.
- GI lymphoma, Inflammatory bowel syndrome, and ulcerative colitis
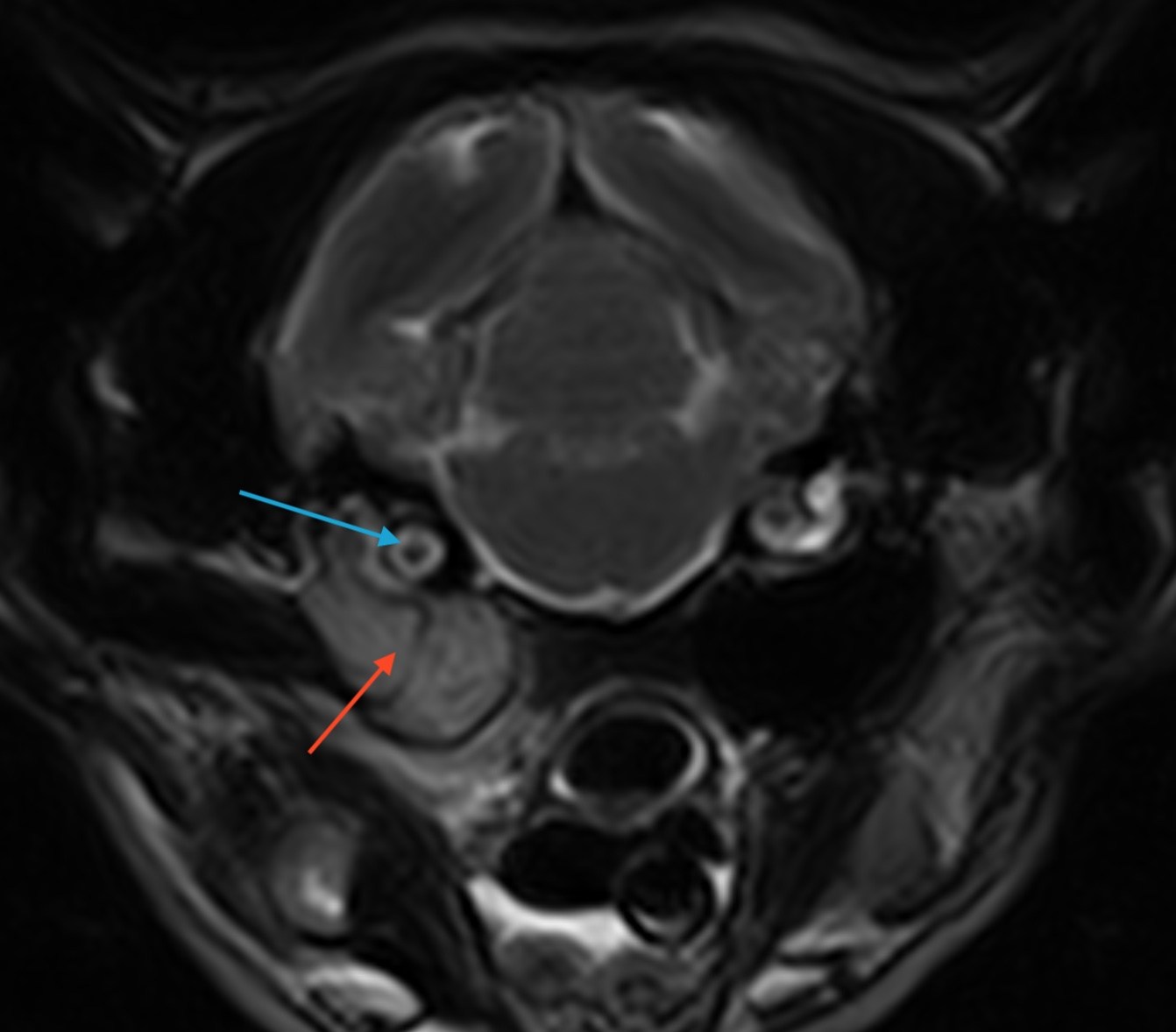
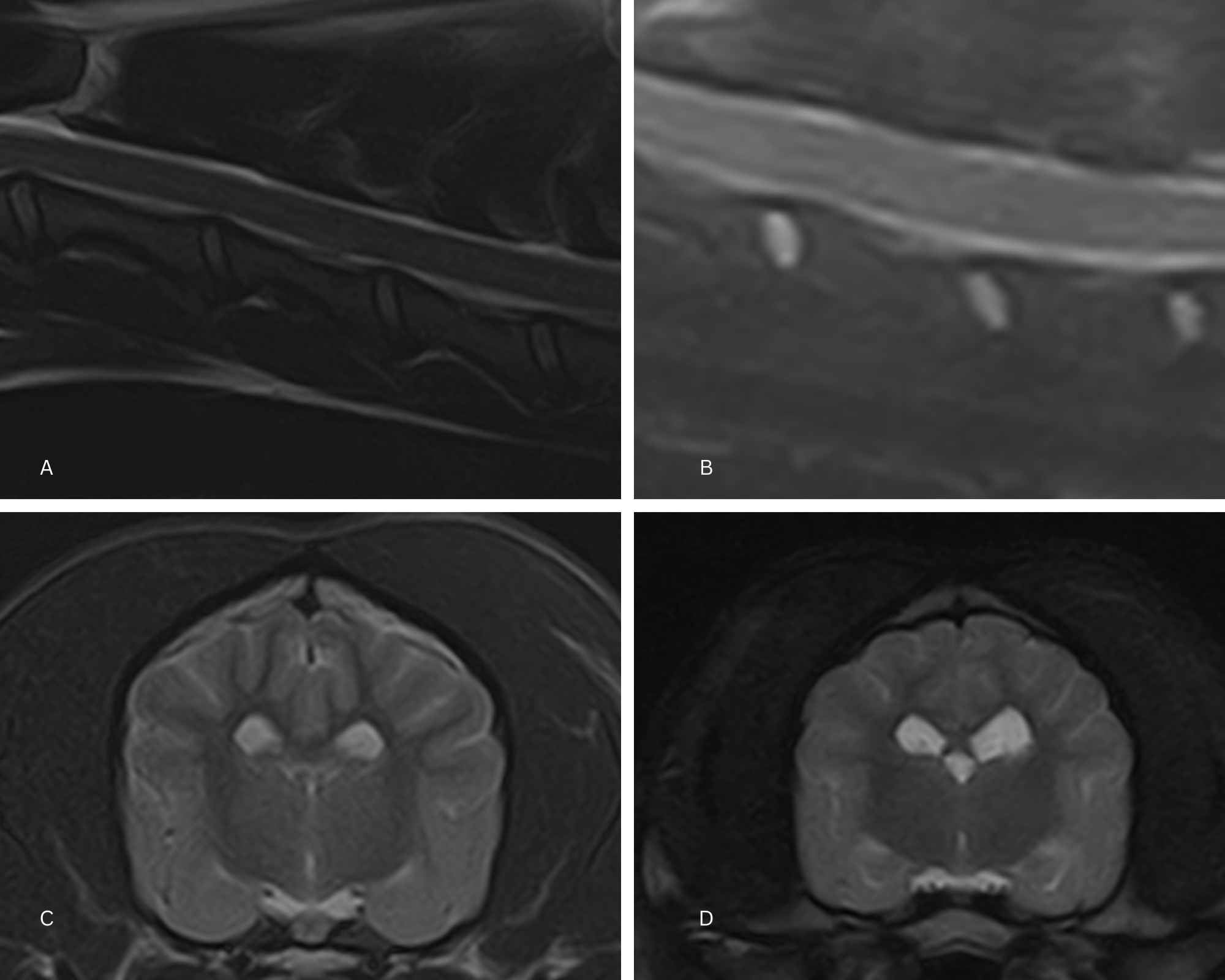
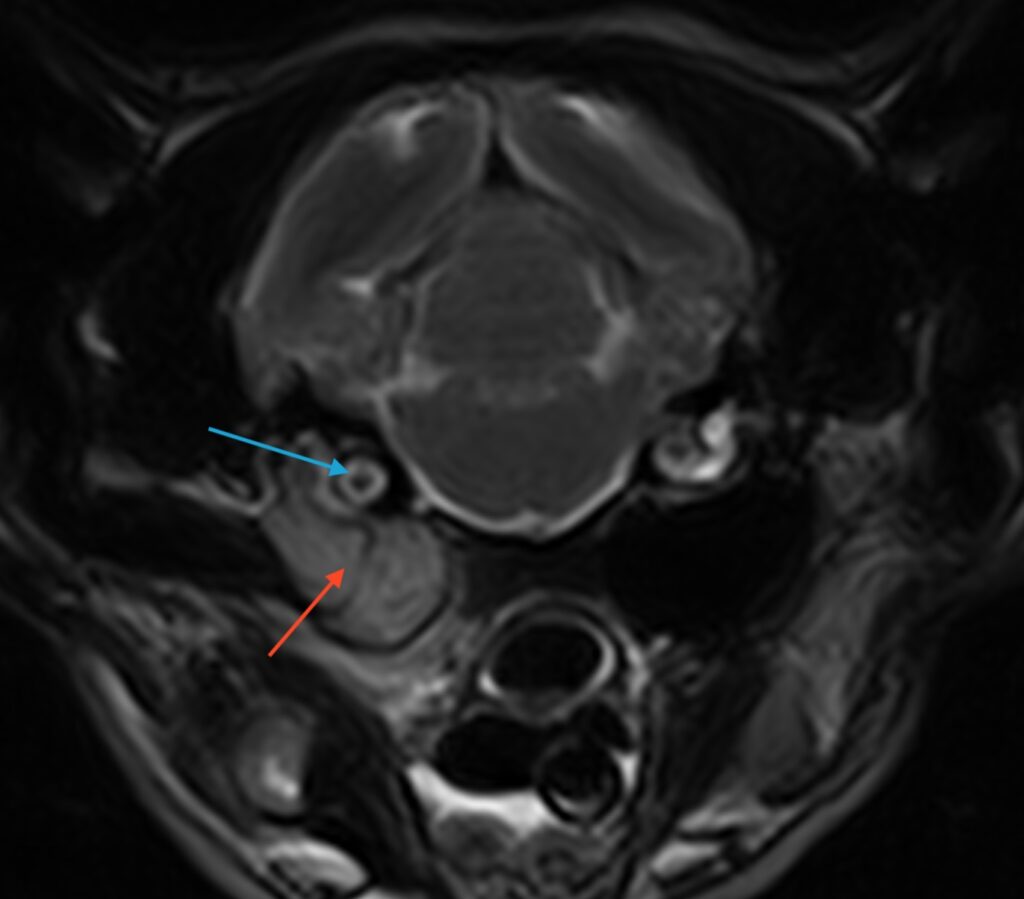
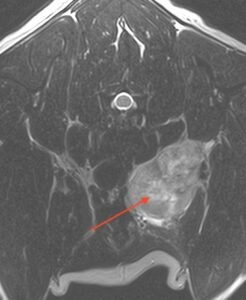
The clinical images below show how MRI enables more targeted diagnostics and therapeutics which lead to a more accurate and effective plan for the patient. The sooner conditions like this are identified, the better the prognosis can be, and the less money is spent on symptomatic therapy in the meantime.
Incorporating these shorter MRI protocols also brings cost savings for the pet owner. Take a look at the scenarios below that illustrate the difference:
Scenario one: traditional route to diagnosis
Patient A is seen for vomiting and inappetence. Radiographs and ultrasound are inconclusive for an obstruction or foreign body. Other considerations include ileus from gastroenteritis. Intravenous fluids and overnight hospital stay is recommended with repeat radiographs after 12-24 hours. Vomiting has progressed to regurgitation – although radiographs and ultrasound do not conclude obstruction or obvious foreign body, these diagnostics are supportive of little response to treatment. Discussion is made to proceed with exploratory surgery. A foreign body was found in the small intestines as well as compromised intestinal segments; resection and anastomosis are performed.
We can expect the costs to be in the region of:
- $5650; Hospital stay – 72 hours.
- $750 for radiographs/review
- $800 in treatment and overnight hospitalization
- $100 Abdominal US FAST scan
- $250 repeat radiographs
- $2700 Exploratory surgery/anesthesia
- $450 for resection and anastomosis
- $600 post-operative care and medications to go home
An estimated total cost of around $11,300 makes this route to diagnosis unfeasibly high for the pet owner. In addition, it places high demands on practice staff and resources. In comparison, scenario two illustrates the difference in both cost and time for practice and patient when MRI short protocol is used:
Scenario two: MRI short protocol for diagnosis
Patient B is seen for vomiting and inappetence. An MRI short protocol is performed and confirms foreign body. The patient is already under propofol anesthesia and is transferred to inhaled anesthesia for surgery which is performed within 1 hour of presentation. Because of early intervention, only an enterotomy is needed to remove the obstruction. The patient is recovered and discharged within 24 hours after presentation.
We can expect the costs to be in the region of:
- $4300; Hospital stay 24 hours.
- $750 for short protocol MRI
- $2700 Exploratory surgery/anesthesia
- $250 for enterotomy
- $600 post-operative care and medications to go home
In conclusion, early accurate detection in this scenario resulted in a saving of $2,700 along with a reduction in severity of condition, a simpler medical intervention, and a significantly shorter hospital stay for the pet who can return home within 24 hours.
About the author:

Dr. Love, DVM, graduated from the University of Wisconsin-Madison, College of Veterinary Medicine in 2004 after which she completed a Doctorate at the Leibniz Institute for Zoo and Wildlife Research, Berlin, Germany. She was an Alexander von Humboldt post-doctorate fellow and participated in a research stay at Erasmus Medical Center in the Netherlands. Catherine became the Interim Director of Veterinary Technology at LaGuardia Community College in NY while working at the Eastside Animal Hospital as an Associate Veterinarian and becoming the Head Vet at Haute Vet and Veterinary Relief Services. Dr. Love was the Chief Veterinary Officer at the Center for Comparative Physiology at the Feinstein Institute in NY from 2014 to 2016 after which she transitioned to emergency medicine. In this role, she served as an ER clinician in Louisiana, Maine, North Carolina and was Director of Veterinary Services at Arkansas Veterinary Emergency & Specialists. Catherine completed an MBA at the Quantic School of Business and Technology in 2022 and recently joined the Veterinary Emergency Group travel team.
INTERESTED IN VISIONARY VETERINARY IMAGING?