Repeat MRI scans are a valuable tool for tracking the progression, regression, or resolution of neurological disease. Just as repeated clinical examinations help monitor a patient’s condition over time, serial imaging can reveal critical changes in disease activity and treatment response. Despite its potential, the role of follow-up imaging remains underrepresented in the literature. While recent studies highlight its importance, there is still a clear need for more prospective research. In this post, guest author Koen Santifort, DVM, MSc (Hons), Dip. ECVN, IVC Evidensia Lead Neurologist, explores the current evidence and presents two case studies where repeat MRI was key to diagnosis.
From image to insight: how MRI studies guide us
With the increased access to and possibility of performing advanced diagnostic imaging studies in veterinary patients, literature on, for instance, magnetic resonance imaging findings in dogs and cats with neurological disorders has boomed in recent years. Most of these reports have confirmed diagnoses based on for example genetic tests or histopathology or alternatively their conclusions are based on adequately supported presumptive diagnoses. These reports provide clinicians around the globe with important information for the MRI based diagnosis of disease in the patient on which further diagnostic tests, treatment, and prognoses are based.
Why repeat imaging studies can make all the difference
However, the value of following the progression, regression, combination thereof, or resolution of disease based on imaging studies is relatively scarcely represented in literature to date. Fortunately, the value of repeated imaging seems to be reflected in some of the recently published papers. Still, a big knowledge gap remains where prospectively designed follow-up imaging studies are needed to highlight the use (or lack thereof) for the importance of repeat MRI (or other modality) studies. Alternatively, it may be that while studies can provide evidence for the usefulness of repeat imaging, research can also help us to decide when repeat imaging may not be indicated.
There are several aspects to consider where the value of repeat imaging studies is concerned.
Monitoring disease progression and therapy response
Repeat MRI scans enable clinicians to monitor the evolution of lesions over time. Take the value of a good clinical neurological examination and repeating that examination at different time-points to follow the course of clinical disease. Likewise, repeat imaging can provide critical information on disease progression or relapse and treatment effectiveness or lack thereof.
Case example
A four-year-old female castrated Jack Russell Terrier was presumptively diagnosed with meningoencephalitis of unknown origin and treated with immunosuppressive medication for the period of 5-months with complete resolution of clinical signs (still receiving treatment when repeat imaging was performed in tapered dosage according to protocol). Repeat imaging was scheduled in advance for after this 5-month period. Despite the lack of clinical signs at the time of repeat imaging, the MRI study identified previously non-affected sites and new contrast-enhancing lesions.
Detecting new or reactivated lesions
In direct link to the former and in particular, inflammatory lesions can appear or ‘reactivate’ after initial diagnosis, especially if relapse occurs beyond certain timeframes. One study showed that dogs experiencing relapse after approximately 233 days since their first MRI invariably exhibited new or reactivated lesions, whereas those with earlier relapses often did not. This knowledge helps us to decide, early or late in the course of the treatment, to add to the current treatment plan or take a whole different route.
Guiding treatment decision-making
Identifying resolution of disease (e.g. spinal epidural empyema) on repeat MRI while recognising persistent clinical deficits may help to support a decision of halting further medical (antibiotic) treatment. In case of post-surgical imaging, assessing the extent of tumour removal may provide immediately useful information on which to guide emphasis of the importance of post-surgical additional treatment modalities such as radiotherapy.
Changes relating to disease or treatment
The difficulty of relating changes in repeat imaging studies compared to earlier imaging studies is that not only the disease process itself but also the treatment that was initiated since might have its influence on the new reality (that is: the repeat imaging study findings). A recent study identified signs of brain atrophy in dogs with meningoencephalitis of unknown origin on repeat MRI. Whether or not this was due to the disease process or the treatment of immunosuppressive medications including prednisone cannot be concluded with certainty. However, differences between patients with or without such brain atrophy, clinically or otherwise, and differences between patients treated with protocol A versus B are of increased interest merely by this now documented observation.
Clarifying differential diagnosis in ambiguous cases
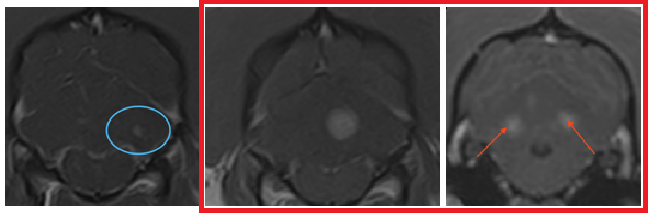
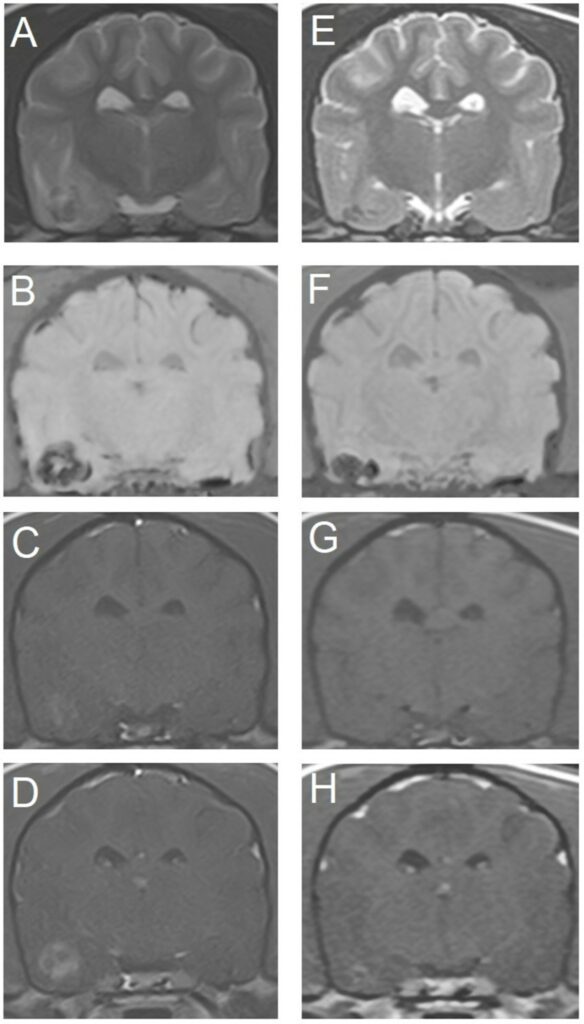
Initial MRI scans may yield inconclusive results and lead to the inability to differentiate with certainty between diagnostic categories such as inflammation, neoplasia or haemorrhage. Follow-up imaging, including sequences like gradient-echo/susceptibility weighted imaging, can reveal distinct temporal patterns. For example, characteristic signal evolution in haemorrhage versus tumour tends to become evident on repeat scans, helping to differentiate benign haemorrhagic haematoma from haemorrhagic neoplasms. The value of repeat imaging in intracranial strokes in dogs was emphasised in an earlier blog.
Case example
Transverse magnetic resonance images of the brain of an 11-year-old miniature Dachshund with a primary haemorrhagic encephalopathy – idiopathic haemorrhagic stroke. All images are at the level of the temporal lobes and caudal aspect of the interthalamic adhesion. Left is on the right of the images. A–D are images from a study 3 days after peracute onset of clinical signs. E–H are images from a follow-up study performed 4 weeks later. (A,E) T2-weighted. (B,F) Susceptibility-weighted. (C,G) T1-weighted. (D,H) T1-weighted post-contrast.
From: Santifort KM, Platt S. Hemorrhagic encephalopathies and myelopathies in dogs and cats: a focus on classification. Front Vet Sci. 2024 Oct 28;11:1460568. doi: 10.3389/fvets.2024.1460568.
Challenges and changes
There are challenges associated with repeat imaging studies, including associated costs, availability (i.e. a single institution may be underequipped to offer repeat imaging to patients in favor of performing studies in patients for the first time, logistically), and anaesthetic procedure risks. Technical developments and studies providing evidence for the usefulness of particular sequences can help to mitigate some of these concerns by, for instance, reducing scanning time. Hopefully, such developments can help to make repeat imaging studies more feasible and cost-effective, for clinicians, clients/owners, and patients.
References
- Blanco C, Moral M, Minguez JJ, Lorenzo V. Clinical Presentation, MRI Characteristics, and Outcome of Conservative or Surgical Management of Spinal Epidural Empyema in 30 Dogs. Animals (Basel). 2022 Dec 17;12(24):3573. doi: 10.3390/ani12243573.
- de Freitas MI, Vettorato E, Scarpante E, Cherubini GB, Caine A. Retrospective Preliminary Assessment of Routine Follow-Up Low-Field Magnetic Resonance Imaging in Dogs Presumptively Diagnosed With Discospondylitis. Front Vet Sci. 2022 May 18;9:880038. doi: 10.3389/fvets.2022.880038.
- Gonçalves R, Walmsley G, Maddox TW. Brain Atrophy in Dogs With Meningoencephalitis of Unknown Origin. J Vet Intern Med. 2025 Jul-Aug;39(4):e70095. doi: 10.1111/jvim.70095.
- Santifort KM, Platt S. Hemorrhagic encephalopathies and myelopathies in dogs and cats: a focus on classification. Front Vet Sci. 2024 Oct 28;11:1460568. doi: 10.3389/fvets.2024.1460568.
- Soulé C, Blond L, Cavalerie R, Piazza S, Baudin-Tréhiou C. Evolution of Brain Magnetic Resonance Imaging Lesions in Dogs Treated for Meningoencephalomyelitis of Unknown Origin Between Initial Diagnosis and Relapse. J Vet Intern Med. 2025 May-Jun;39(3):e70086.