Equine solar penetration is a potentially serious and life-threatening injury that is commonly seen in equine practice. Guest author Connie Bowkett-Pritchard BVSc PG Cert (VetMed) PG Cert (VPS) CertAVP (EL) MRCVS, describes the use of Magnetic Resonance Imaging (MRI) for the assessment of such injuries. She considers suitable scanning protocols and their possible limitations and reviews available literature regarding injury prognosis.
Why MRI for equine solar penetration injuries?
The aim of diagnostic investigations is to promptly ascertain which intracapsular anatomy has been affected. The nail has often been removed by the time the horse receives veterinary attention. However, it is extremely important to understand the site of entry, depth and direction of the penetrating object. Clinically, it can also be difficult to see the penetration site in the solar surface if the location is not known or documented. Injuries to the central or palmar/plantar frog warrant suspicion of synovial sepsis (1).
Potential synovial structures affected are the distal interphalangeal joint (DiPJ), the navicular bursa and the digital flexor tendon sheath. Where penetration into the DiPJ has occurred, by default, the deep digital flexor tendon (DDFT), in addition to the distal sesamoidean impar ligament, will have sustained damage. A study of synovial penetrations in multiple UK equine hospitals reported the DDFT, DIPJ and navicular bursa as most commonly affected (1).
Why diagnostic imaging is crucial in directing treatment
The gold standard treatment for synovial sepsis is endoscopic lavage under general anaesthesia (2) as well as debridement of damaged tendinous and or ligamentous tissue. In contrast, if these structures are unaffected, cases can normally be managed with local debridement.
Diagnostic imaging is crucial to directing the treatment plan for equine solar penetration injuries which have significant cost implications for the owner.”
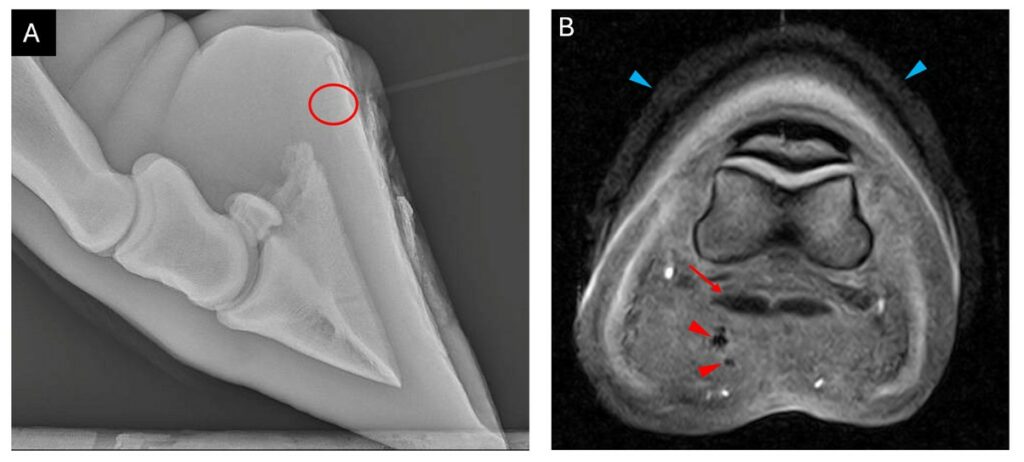
Radiographs can be useful to assess the tract and evaluate osseous pathology however visualisation of the tract (Figure 1) is not always possible. In a study of navicular bursa puncture, 66% of cases did not show any radiographic abnormalities on initial presentation (3).
Transcuneal ultrasonography has been reported in a foot penetration in a young foal (4) but is often unrewarding in adult horses due to poor penetration of the hoof capsule by ultrasound waves (5).
MRI protocol for equine solar penetration injuries
To ensure patient comfort and compliance, appropriate analgesia should be administered to patients prior to scanning if this has not already been done prior to referral. An abaxial sesamoid nerve block using bupivacaine (for its longer duration of action) may also be appropriate to reduce motion artefact.
Placement of a hoof bandage soaked in water permits visualisation of the hoof capsule (6). To the author’s knowledge, whether this improves diagnostic capabilities is yet to be investigated.
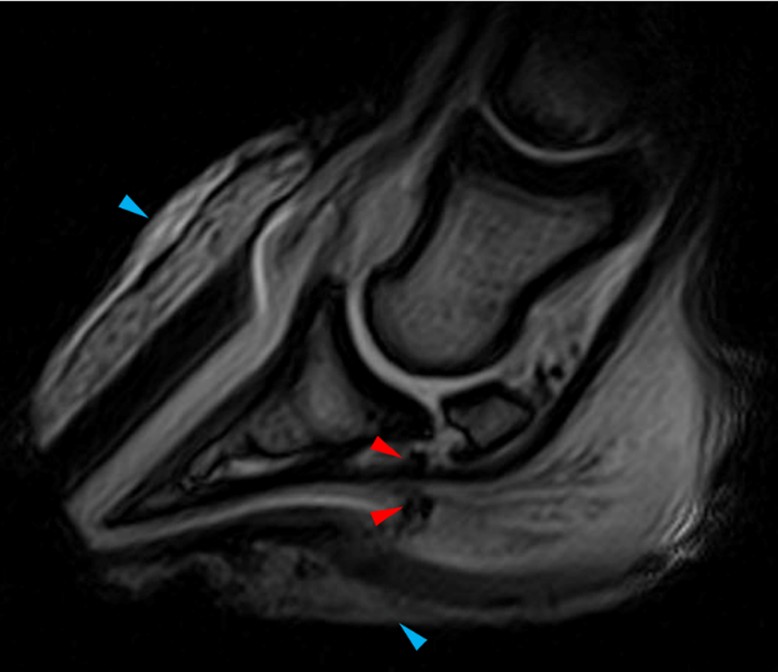
Orthogonal planes allowing the tract to be followed should form part of the MR examination. If the tract is visible, a protocol focusing on the tract can be used, reducing the number of scans required compared to a standard foot study. A T2* sequence and a transverse image plane have been shown to produce the greatest lesion conspicuity (7) and therefore should form part of the imaging protocol. T2* sequences can identify haemorrhage which appears as regions of susceptibility artefact due to haemosiderin causing magnetic field inhomogeneities (7,8) (Figure 2). Gradient recall echo sequences are also advantageous due to their shorter acquisition time compared to spin echo sequences.
In cases of tendinous or ligamentous pathology, a repeat MRI is warranted to assess the full extent of damage as well as to monitor healing. False negative diagnoses of DDFT injury have been reported in the first 48 hours post injury (9).
MRI findings
MRI can visualise the extent of the penetrating tract and identify the structures involved (10). The tract normally appears as an irregular region of signal void or hypointensity (7) on all sequences extending from the sole (Figures 1 and 2). MR examination of recent injuries (less than one week) is more likely to identify a tract compared to more chronic injuries (7). Reported injuries to the DDFT include linear hyperintensities and core lesions (7). Comparison between surgery and MRI identified correlations in the navicular bursa or in the palmar/plantar border of the DDFT, at the sesamoidean level (7).
Limitations of MRI when examining solar penetration injuries
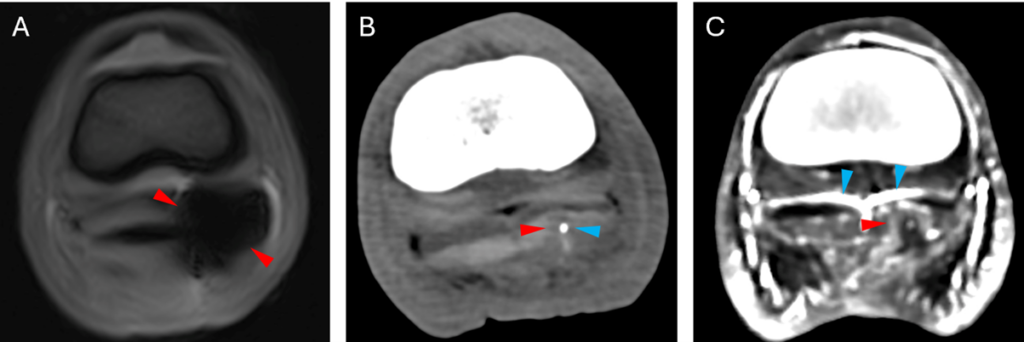
Certain circumstances can inhibit the use of MRI to examine solar penetration injury. Foreign material cannot always be identified; del Junco and colleagues reported 2 horses with wood identified at surgery that was undetected on MRI. This corroborates a more recent study by Ogden et al (11) who found that CT provides higher visibility of foreign material within the foot compared to MRI.
Despite its use in tract detection, haemosiderin, as well as residual foreign material, can preclude the identification and or cause distortion of anatomical structures due to susceptibility artefact (1,8). Metallic fragments can remain in a tract despite removal of a penetrating object; this may be detectable radiographically prior to MRI. In such instances, appropriate communication with the owner is important to inform them of potential limitations of the MRI examination. In such instances, CT can be used to visualise the tract (4) and the addition of contrast can aid identification of damage to the DDFT (Figure 3).
Prognosis
A critical appraisal evaluating the use of MRI in foot penetration injuries cites the need for further research into the value of MRI in prognostication of solar penetration injuries (10). However, limited information is available.
In del Junco’s study, the decision to euthanise horses was made on clinician judgement depending on the use of the animal and expectations and financial considerations of the owner. The study recorded that 50% of those with injury between the DDFT insertion and the palmaroproximal aspect of the distal phalanx, and 22% of those with injury between the palmaroproximal aspects of the distal and middle phalanges, were euthanised.
A retrospective series of 11 horses with solar penetration and DDFT injury, free of synovial sepsis, reported 60% returned to full athletic function while 40% were sound but had not yet resumed work (12). In contrast, in a study of 95 horses with solar penetration and synovial sepsis that underwent surgery, 56% survived to hospital discharge and 36% regained previous athletic function. Increasing days to presentation, direct penetration of the central frog sulcus and distal phalanx injury were associated with euthanasia during hospitalisation. Increasing days to presentation and a patient undergoing more than one surgery was also associated with failure to return to pre-injury level. The authors also acknowledged that return to pre-injury athletic function is likely related to the horse’s work level.
Another study of solar penetrations within the central foot found that 29% of equids with synovial structure involvement regained soundness but overall, 60% of affected patients became sound. Early treatment and involvement of a hindlimb were associated with a more favourable outcome (13).
Conclusion
MRI provides an important means of distinguishing between equine solar penetrations that involve synovial structures and those in which these structures are avoided as well as assessing damage to soft tissue structures, especially the deep digital flexor tendon. The literature suggests the involvement of synovial structures has an important influence on the horse’s prognosis and supports prompt treatment of such cases.
References
- 1. Findley JA, Pinchbeck GL, Milner PI, Bladon BM, Boswell J, Mair TS, et al. (2012) Outcome of horses with synovial structure involvement following solar foot penetrations in four UK veterinary hospitals: 95 cases. Equine Vet J. 46(3):352–7.
- 2. Wright IM, Smith MRW, Humphrey DJ, Eaton-Evans TCJ and Hillyer MH (2003) Endoscopic surgery in the treatment of contaminated and infected synovial cavities. Equine Vet J. 35(6):613–9.
- 3. Richardson GL and O’Brien TR (1985) Puncture Wounds into the Navicular Bursa of the Horse. Vet Radiol. 26(6):203–7.
- 4. Bowkett-Pritchard C and Baldwin CM. (2024) Comparative imaging of septic navicular osteomyelitis caused by a solar penetration injury in a 15-day-old Shire foal. Equine Vet Educ. 36(8):431–7.
- 5. Jacquet S and Denoix JM. (2012) Ultrasonographic examination of the distal podotrochlear apparatus of the horse: A transcuneal approach. Equine Vet Educ. 24(2):90–6.
- 6. Mair TS and Linnenkohl W (2012) Low-field magnetic resonance imaging of keratomas of the hoof wall. Equine Vet Educ. 24(9):459–68.
- 7. Urraca Del Junco CI, Mair TS, Powell SE, Milner PI, Font AF, Schwarz T, et al. (2012) Magnetic resonance imaging findings of equine solar penetration wounds. Vet Radiol Ultrasound. 53(1):71–5.
- 8. Murray, R.C. and Werpy, N. (2011) Image interpretation and artefacts. In: Equine MRI, 1st edn Ed: Murray, R.C. Wiley Blackwell, Chichester, pp. 101-146.
- 9. Kinns J and Mair TS. (2005) Use of magnetic resonance imaging to assess soft tissue damage in the foot following penetrating injury in 3 horses. Equine Vet Educ. 17(2):69–73.
- 10. Meehan L. (2017) Should I use magnetic resonance imaging to evaluate horses with foot penetrations? Equine Vet Educ. 29(9):521–2.
- 11. Ogden NKE, Milner PI, Stack JD, Talbot AM. (2021) CT more accurately detects foreign bodies within the equine foot than MRI or digital radiography. Vet Radiol Ultrasound. 62(2):225–35.
- 12. Schiavo S, Cillán-García E, Elce Y, Liuti T and Taylor SE. (2018) Horses with solar foot penetration, deep digital flexor tendon injury, and absence of concurrent synovial sepsis can have a positive outcome. Vet Radiol Ultrasound. 59(6):697–704.
- 13. Kilcoyne I, Dechant JE, Kass PH and Spier SJ. (2011) Penetrating injuries to the frog (cuneus ungulae) and collateral sulci of the foot in equids: 63 cases (1998-2008). J Am Vet Med Assoc. 239(8):1104–9.







