For cats and dogs, severe head trauma causing traumatic brain injury (TBI) is associated with high mortality rates. In order to increase the chance of recovery to a level that is both functional and acceptable to the owner, treatment of affected animals must be immediate. Dr. Simon Platt, Hallmarq’s Small Animal Medical Director considers the causes, diagnosis, and prognosis and looks at how imaging of the patient is invaluable in the assessment and management of patients with TBI.
Common causes of head trauma
Common causes of head injuries in cats and dogs include road traffic accidents, falls, kicks, gunshot or pellet wounds, and bites from larger animals. As with all types of acute injury, the ‘ABC’ (airway, breathing, circulation) of emergency care is extremely important. The initial physical assessment of the severely brain-injured patient focuses on imminently life-threatening abnormalities. Additionally, a neurological assessment should be performed and repeated every 30–60 minutes to assess prognosis and monitor the efficacy of any therapies administered.
Where does imaging of the patient fit into this approach?
Imaging of the patient’s head is indicated in animals that fail to respond to aggressive medical therapy or deteriorate after an initial response. Skull radiographs are unlikely to reveal clinically useful information about the brain injury but may occasionally reveal evidence of skull fractures. These should never be interpreted in isolation from the neurological examination.
Can CT help with prognosis and treatment options?
CT is a rapid, relatively cheap, and highly accurate method for the detection of intracranial haemorrhage or skull fracture. A full-body CT performed once the animal has been stabilized can provide information about intracranial injuries as well as systemic injuries, without the need to rotate the patient for additional views, and may be similar in cost to multiple radiographic projections.
Abnormal CT findings negatively associated with prognosis for the brain-injured patient include midline shift, high or mixed density parenchymal lesions, presence, shape, and accessibility of intracranial mass, presence of intra-ventricular or subarachnoid haemorrhage and the status of suprasellar and basal cisterns.
A veterinary medicine scoring system, (the Koret CT score (KCTS)) considers lesions such as cranial vault fractures, haemorrhage, midline shift, ventricular asymmetry, and location of lesions. Each of the mentioned abnormalities is given a score based on its presumed effect on prognosis and is very sensitive in predicting short and long-term survival.
Should MRI be considered instead of CT?
In the subacute and chronic phase of TBI, MRI is preferred over CT because of its superiority in detecting non-haemorrhagic lesions, brainstem injury, and oedema. Furthermore, intracranial lesions that may benefit from surgery (such as haematomas and pneumocephalus) can be accurately identified using advanced imaging. However, because MRI usually requires general anaesthesia, it may not be appropriate for unstable patients.
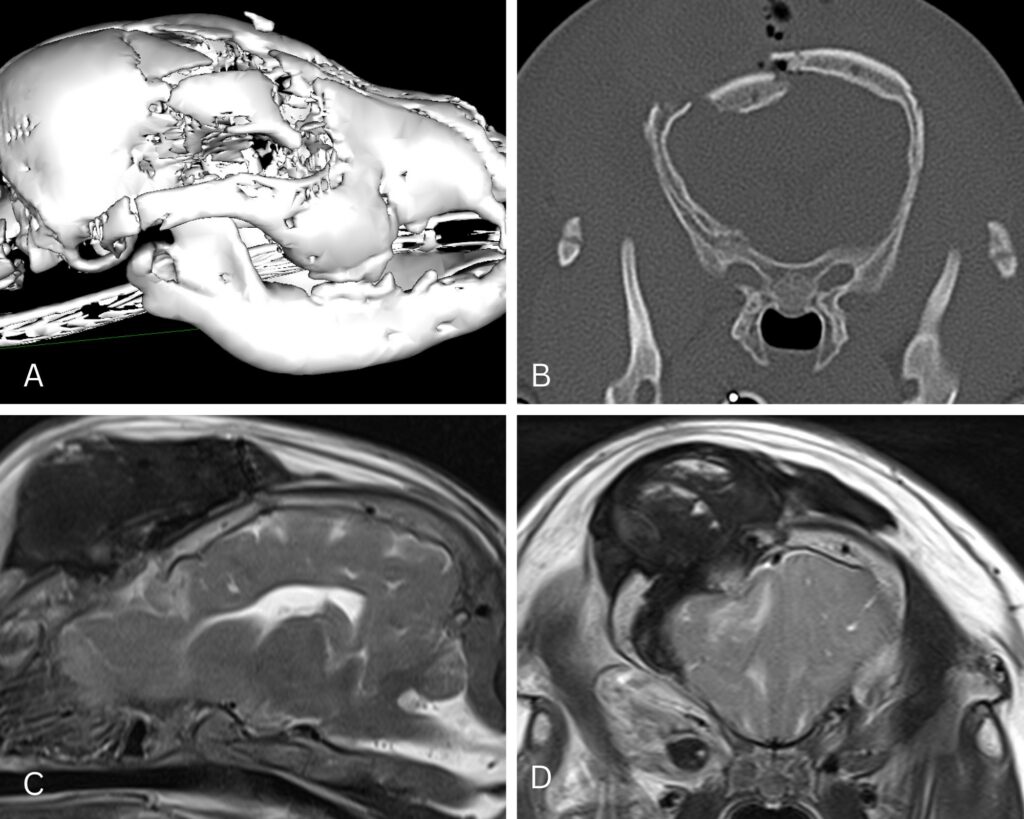
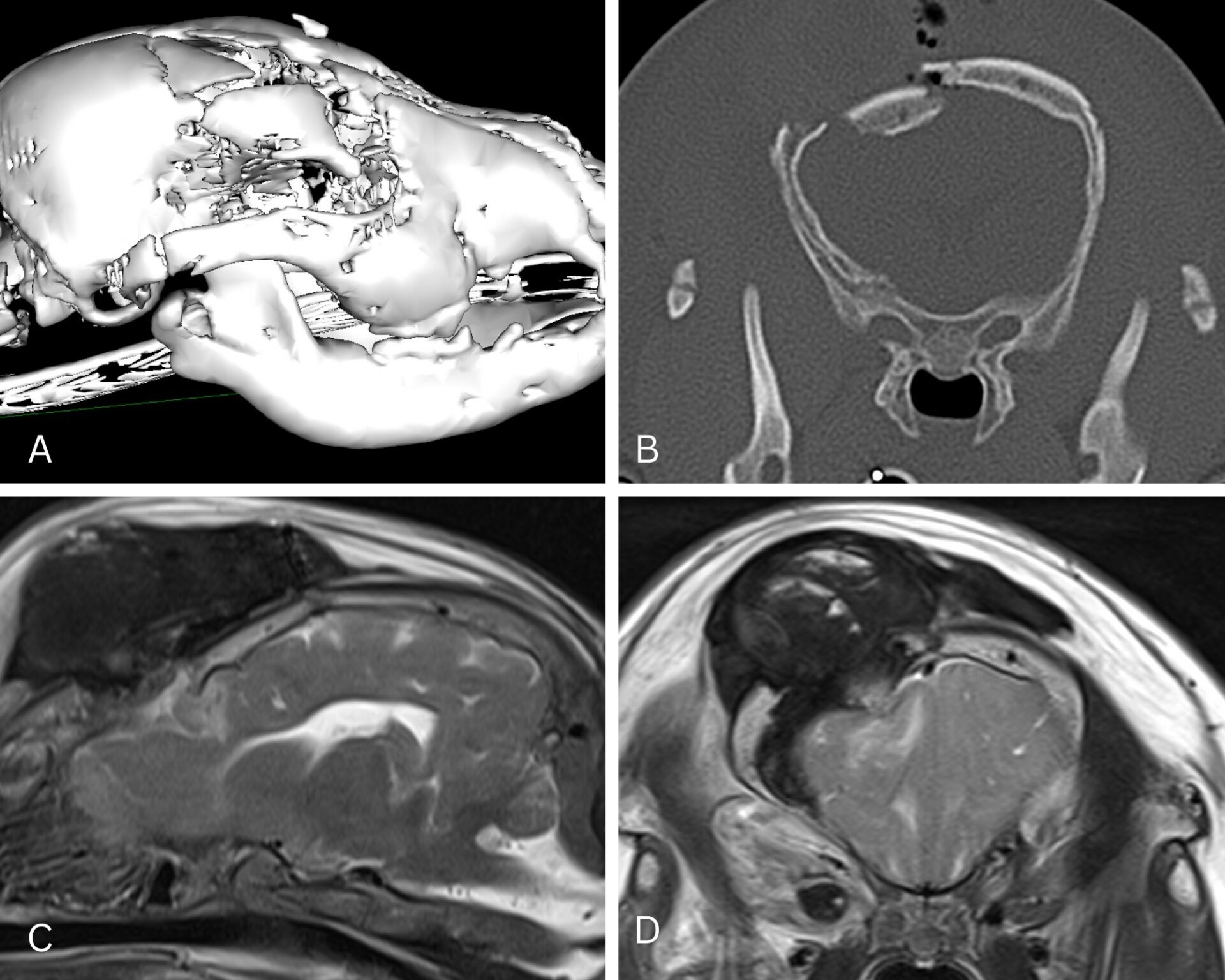
A Great Dane puppy was attacked by another dog and presented with right-sided visual deficits, a dull level of consciousness and seizures. Once the dog. Was systemically stable and had been appropriately medically treated, a CT scan and MRI were performed of the skull.
Figure 1: a 3D (A) reconstruction enables appreciation of a depressed frontal bone fracture which can be seen in transverse section (B). However, this study doesn’t allow a precise evaluation of the underlying brain parenchymal injury, which can be seen to be compressed and exhibiting white matter oedema, on sagittal MRI (T2W) (C) and on transverse MR images (D). Additionally, extracranial soft tissue injuries to the overlying muscles and the retroorbital structures can be seen in (D).
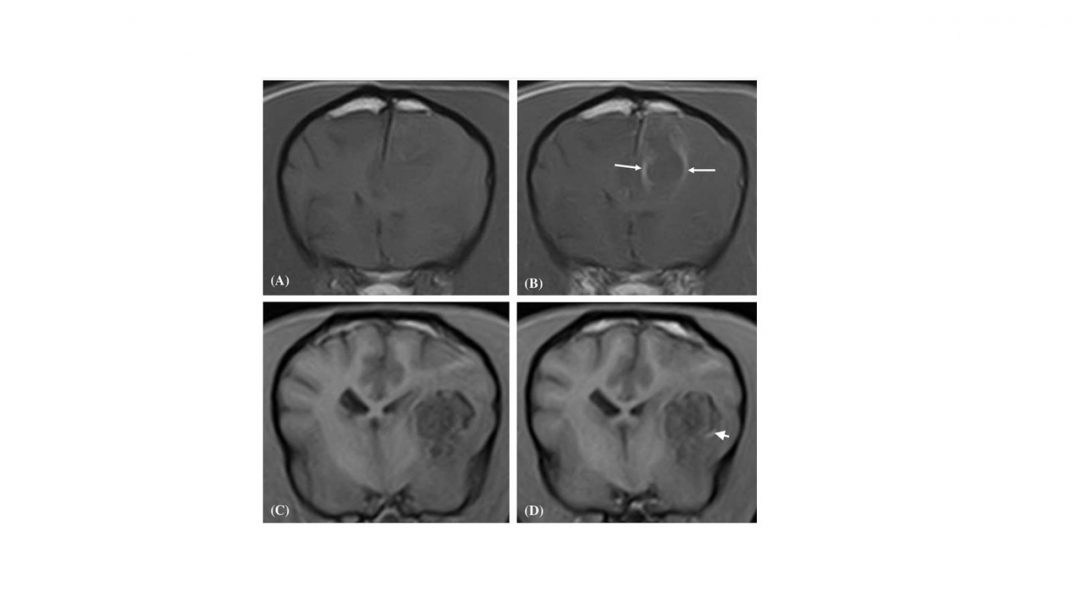
MRI has been shown to provide key information relevant to the prognosis based upon its ability to detect subtle parenchymal damage not evident on CT. The detection of a midline parenchymal shift and ventricular obliteration on MR images are associated with a poor prognosis for survival. A greater area of affected brain parenchyma and a greater degree of midline shift has been associated with poorer clinical outcome. Additionally, the risk of development of post-traumatic epilepsy in dogs has been associated with larger areas of brain damage on MR images.
In conclusion
The role of imaging for the assessment and management of cats and dogs with head trauma is a valuable one. However, it should not take precedence over the systemic stabilization of the patient and its neurological examination, nor should the results be taken in isolation. The stability of the patient should definitely be considered prior to undertaking neurological imaging studies.
Dr. Simon Platt is Small Animal Medical Director with Hallmarq Veterinary Imaging.