Spinal trauma in the small animal patient can be caused by various external events, such as being hit by a car, falling from a height, or a fight with another animal. Guest blogger Samantha Vitale, DVM, MS, DACVIM (Neurology) from virtual specialists Stratocyte, discusses what to consider when imaging the spinal trauma patient.
First things first
When a patient presents with a history suggesting spinal trauma, there are several immediate factors to consider.
- First, assume that there is an unstable spinal fracture or luxation until proven otherwise! Do your best to limit spinal mobility during your initial assessment to prevent further injury.
- Equally as important is a thorough assessment of your patient. Unfortunately, traumatic injuries often affect multiple body systems, so ensuring your patient’s overall health and stability is essential.
- Once your patient is stabilized, perform an abbreviated neurologic exam. Assess their mentation and cranial nerves to look for signs of head trauma. If your patient is recumbent, do not force them into a standing position. To the best of your ability, assess the movement, sensation, and reflexes in all four limbs to help you determine your patient’s prognosis and guide treatment recommendations. This evaluation should be performed with limited manipulation of the spine.
- Finally, as soon as you have had a chance to assess your patient, you should administer analgesia.
Consider your options
There are 3 imaging modalities that can be used to evaluate patients with spinal trauma: radiographs, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI). Let’s take a look at the pros and cons of each one when it comes to small animal spinal trauma.
Radiographs
Pros:
- Fast!
- Anaesthesia is not required
- Great screening tool for fractures and luxations.
Cons:
- Two-dimensional view only
- You cannot evaluate the spinal cord itself on radiographs
- Radiographs are not as sensitive as CT and MRI for spinal fractures and luxations. Approximately 25% of spinal fractures and luxations can be missed on survey radiographs.
- Movement of the patient is often required to obtain 2 orthogonal views
Computed Tomography (CT)
Pros:
- Fastest option for 3-dimensional imaging
- Highest sensitivity for evaluating bone pathology
- A reliable method to detect soft tissue trauma
- In cases of suspected polytrauma, you can easily CT your whole patient to screen for head, thoracic, and abdominal trauma as well as spinal trauma.
- CT is the gold standard for pre-surgical planning when it comes to surgical fixation of spinal trauma, because the high-quality 3D bone imaging allows for measurements and even 3D reconstructions of the images.
Cons:
- May require anaesthesia or heavy sedation, which can be risky in an unstable patient
- While CT provides great detail for many soft tissue structures, you cannot evaluate the spinal cord itself.
- Several traumatic conditions can be missed with CT alone, including intervertebral disc extrusion and spinal cord contusion/hemorrhage.
Magnetic Resonance Imaging (MRI)
Pros:
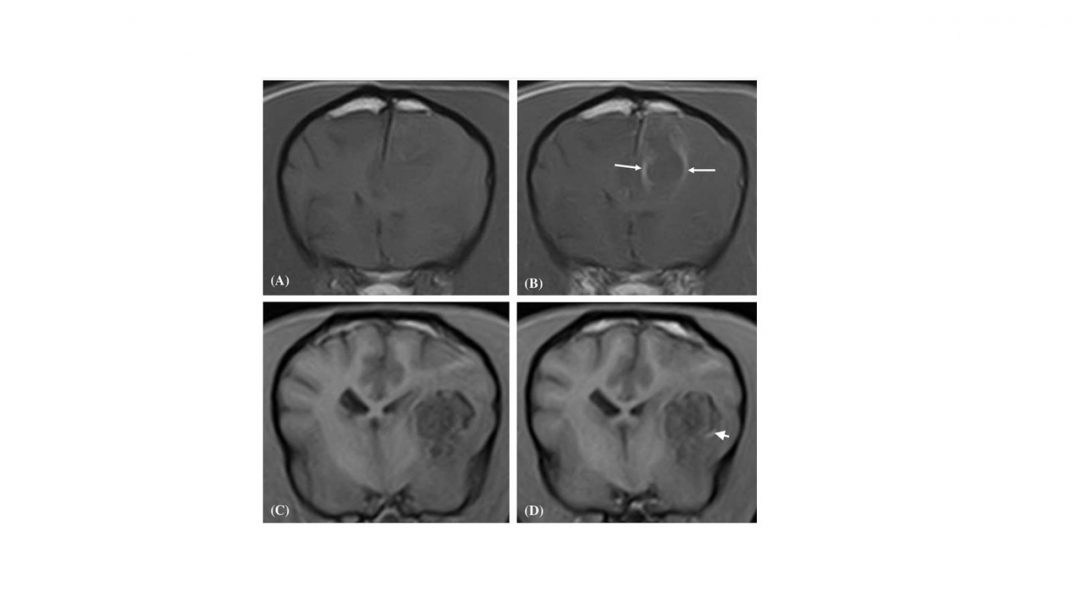
- MRI is the gold standard for evaluating the spinal cord, and it is the most sensitive method for diagnosing non-osseous spinal cord injuries.
- MRI is ideal for evaluating soft tissue injury and is reasonably sensitive for osseous pathology such as fracture/luxation.
Cons:
- MRI requires general anaesthesia and takes the longest of all three methods. This is not ideal for systemically unstable patients.
- MRI images alone may not be adequate for surgical planning for spinal fractures.

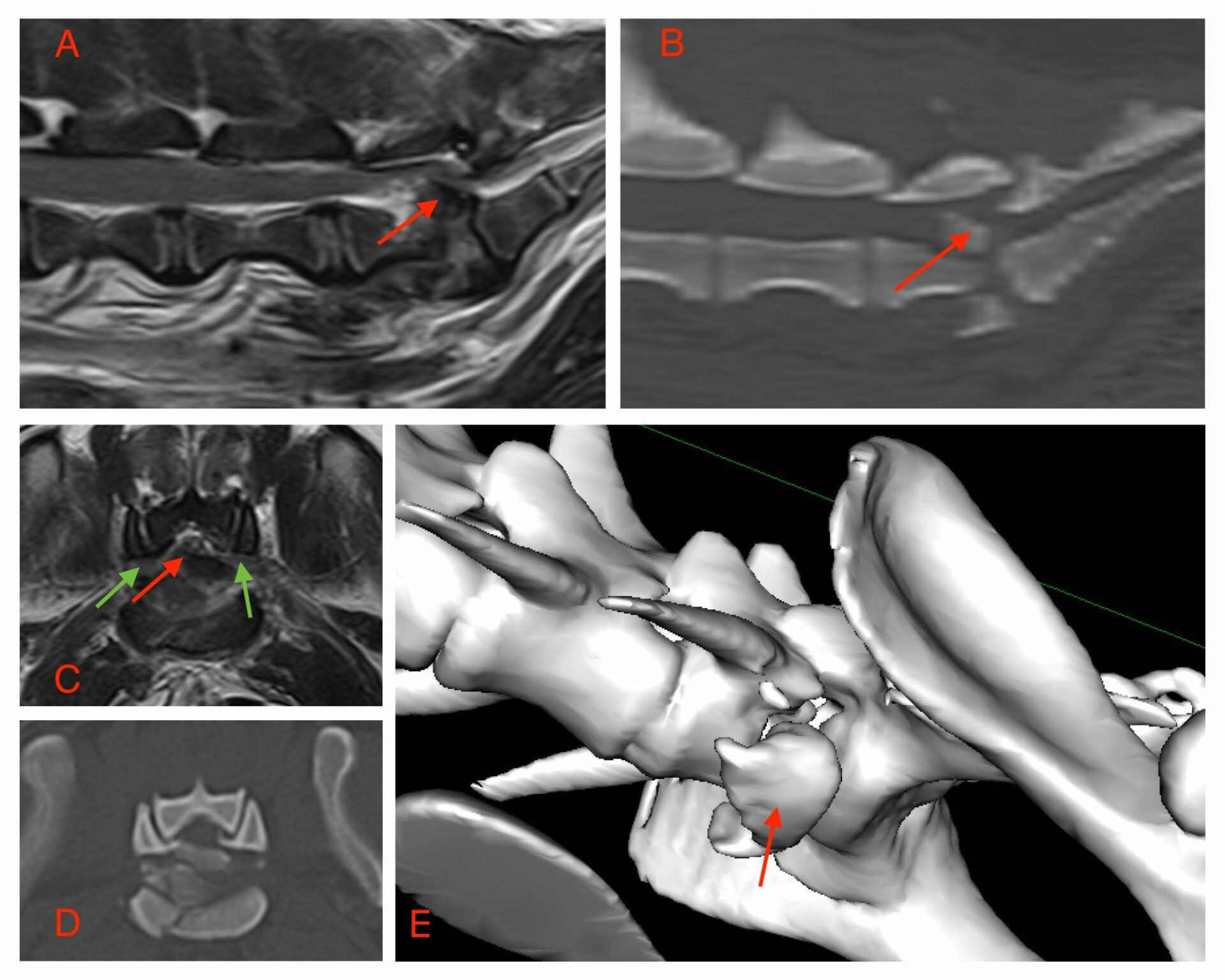
(A) T2W sagittal images demonstrate ventral compression of the caudal cord and conus secondary to a caudo-dorsal displaced fracture of L7 (arrow). The fracture fragments of L7 can be more easily detected on the sagittal reconstructed CT scan (B). A T2W transverse image at L7-S1 reveals the compression of the neural tissue (red arrow) with bilateral swelling of L7 nerve roots within the foramen (green arrows) (C). Detail of the L7 fracture is better seen in the transverse CT image at this level which also reveals minimal subluxation based on the apposition of the facet surfaces (D). A 3D rendered CT (E) allows visualization of the ventral fragment of the L7 fracture
Reducing the risk
Ultimately, more than one of these modalities may be needed to fully determine your patient’s prognosis and best treatment plan. When considering which modality to use first, keep in mind the overall stability of your patient and which option can give you the most information for the least amount of risk!
INTERESTED IN VISIONARY VETERINARY IMAGING?